On this page... (hide)
1. Background
In the U.S. alone, over two hundred thousand individuals are diagnosed with prostate, breast, or liver cancers each year. Increasingly, physicians seek to use non-invasive imaging technologies for real-time guidance in detection and treatment of these cancers. MRI provides physicians with safe, high contrast imaging inside the body that is valuable not only for diagnosis (e.g. of tumors in prostate, breast, and liver) but also procedure planning. Ideally, physicians could conduct surgical interventions with a continuous live view rather than relying on preoperative images. However, this relies on concurrent patient access and imaging, which is largely unachievable with today's technology.
2. Design
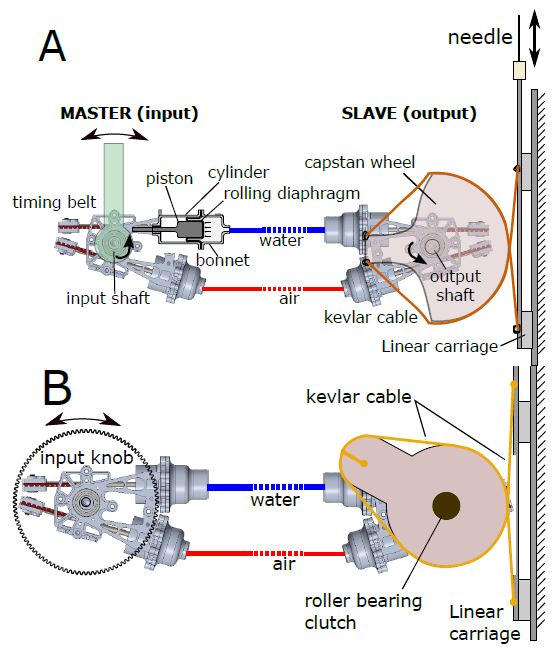
To address this problem we developed an MRI-compatible hydraulic teleoperator that enables remote access to a patient inside an MRI bore with live imaging during tool positioning. The system includes a novel low friction hydraulic transmission and MRI-compatible pneumatic clutch. The transmission utilizes precision ground glass cylinders to achieve nearly frictionless motion. The high stiffness and absence of Coulomb friction allows forces to propagate accurately between the input and output. The clutch enables incremental insertion of a biopsy needle through multiple strokes. This allows the device to fit in the tight space between a patient and the bore wall. Our device is the first system to support MRI guided in-bore liver biopsies with high-fidelity force feedback.
Teleoperation device for in-bore liver biopsies. A physician stands outside the machine, manipulating an input that dictates the motion of a biopsy needle inside the bore.
3. Performance
We conducted experiments in lab and clinical settings to evaluate performance and verify MRI compatibility. We demonstrated negligible impact of the device on MRI scans and a sufficient system bandwidth to enable haptic transparency (force propagation between the input and output with little distortion). Use studies demonstrated that inserting a needle using the teleoperator is as accurate as direct insertion by hand.
Force tracking frequency analysis and sample data at realistic oscillations. Force error between the input and output is <5% and the system bandwidth is near 100Hz.
4. Earlier Work
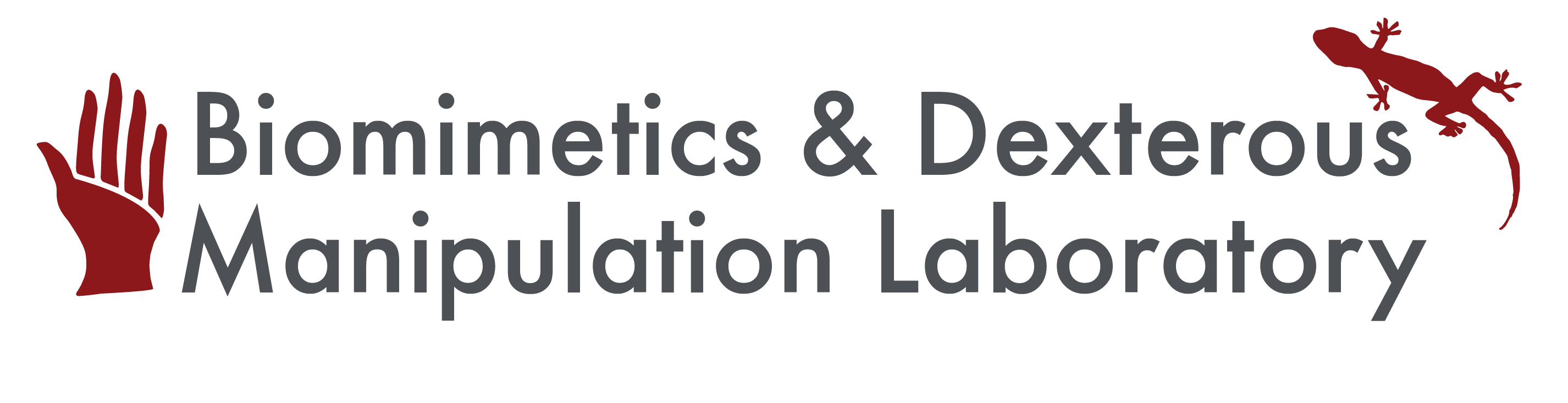
Work on this system began with a rolling-diaphragm hydrostatic transmission. A single water-filled line maintains stiffness and a second, thinner and more flexible line with pressurized air maintains a positive pressure under all conditions. Opposed rolling diaphragm actuators are located at each end and connected via a timing belt to a rotary joint.
|
A) Master and slave sides of the transmission use paired rolling diaphragm actuators. One line is water-filled for stiffness; the other contains pressurized air. The slave side uses a capstan/cable drive to propel the needle on a linear track. |
We conducted experiments against springs to characterize the system performance. The experimental setup and results are shown.
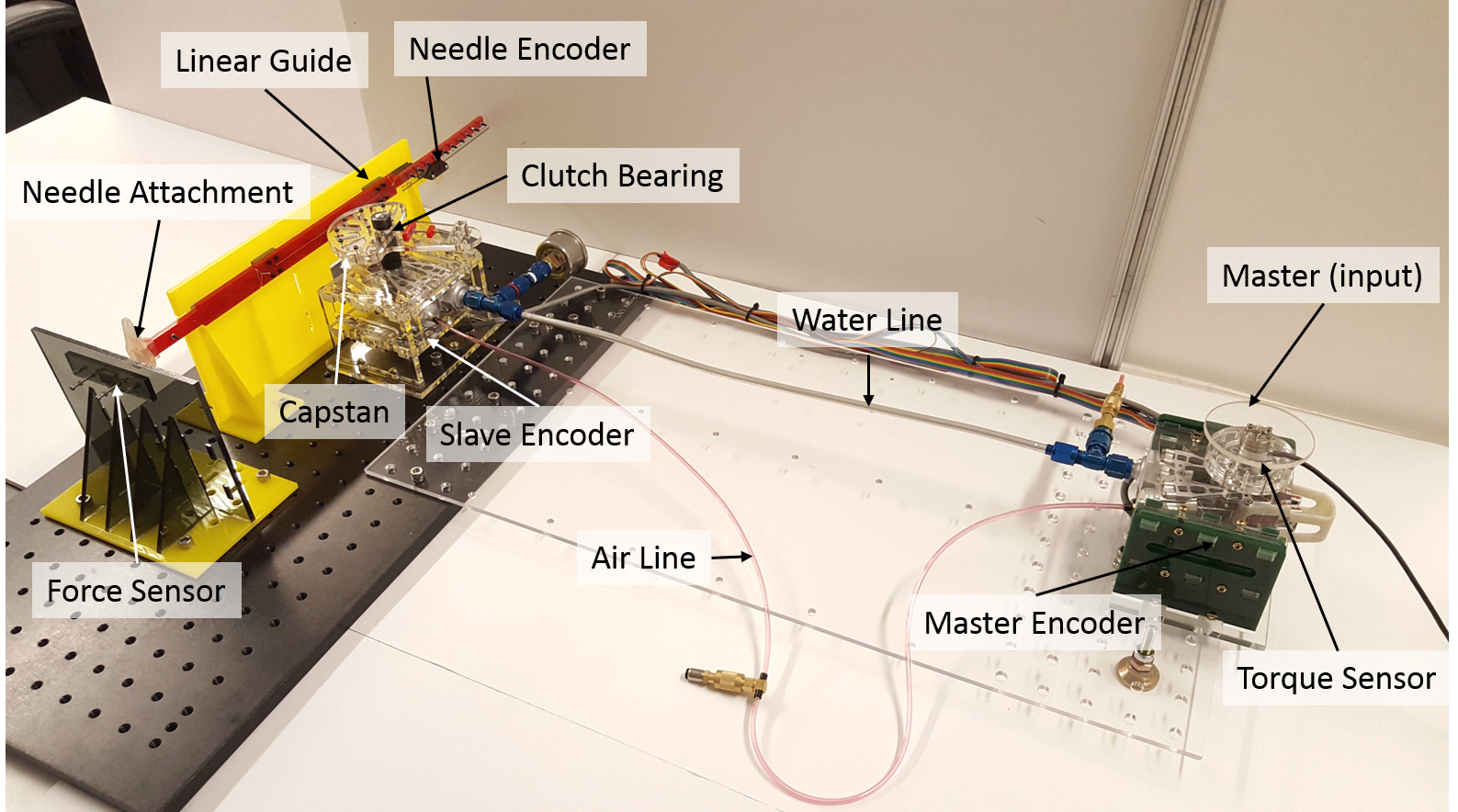
1-DoF transmission system with associated sensors for characterizing force and position transparency. Optical encoders track input and output rotation as well as linear displacement of the needle. Force sensors measure the input torque and force experienced at the needle tip.
-
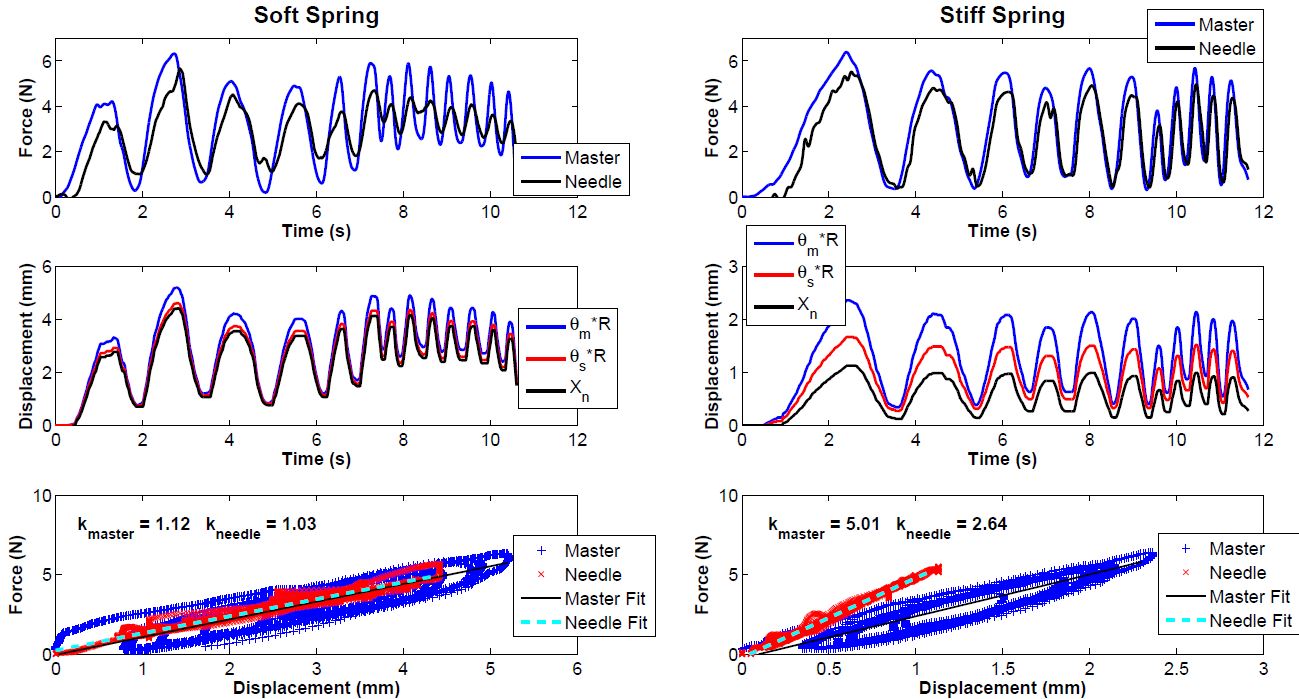
Comparison of system transparency when interacting with soft (A) and stiff (B) springs. Upper row: Changes in force are tracked; magnitudes are expressed with a small lag and higher relative accuracy in the stiff case. Middle row: Displacement errors are approximately equal in the soft and stiff cases. Bottom row: Stiffness as experienced by the input (master) and output (needle). For the soft spring, input stiffness matches endpoint stiffness; for the stiff spring, elasticity in the apparatus contributes noticeably to the apparent stiffness at the master.
-
User tests with phantom tissue were also conducted. The tests measured users’ ability to detect membrane puncture events and to distinguish between different stiffness levels using the teleoperator system versus manipulating the needle directly. Membrane punctures had an average of 77% success (standard deviation was 9%, range = 63-88%). Puncture forces were realistically sized on the lighter end of membranes one would encounter in transperineal prostate biopsy, ranging from 0.31-0.66 N (average = 0.48N, standard deviation 0.10). Users had 100% accuracy in distinguishing all pairs of spring combinations except two: 88% accuracy in distinguishing 2.86 N/mm and 1.54 N/mm, and 63% accuracy for 0.82 N/mm and 0.57 N/mm.
5. Custom Long Stroke Rolling Diaphragms
This has become enough of a project that it gets its own page: LongStrokeRollingDiaphragms
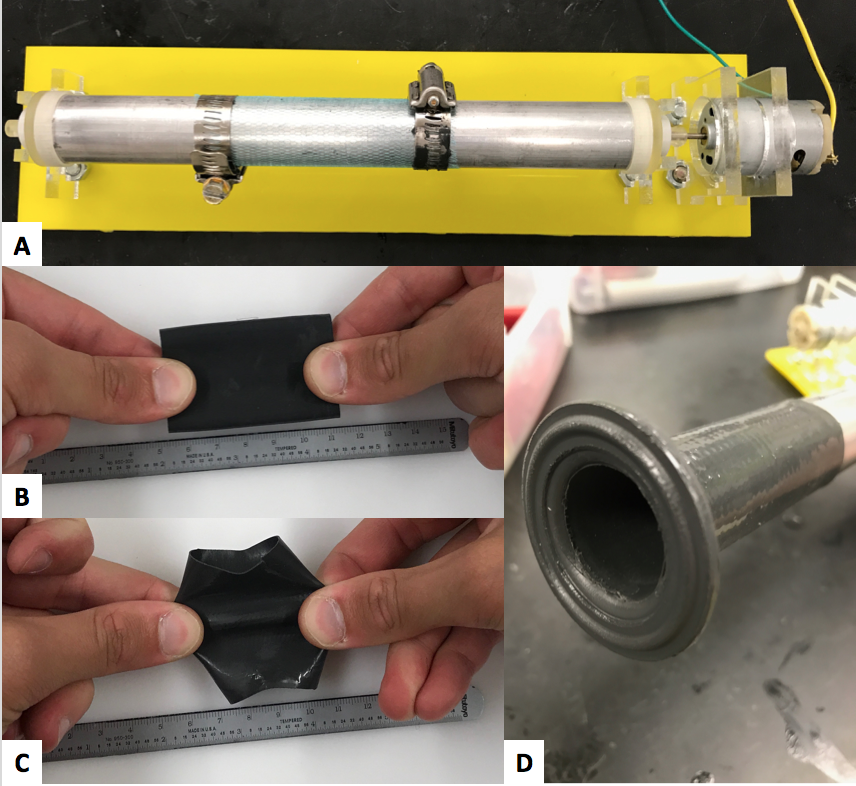 |
One approach used to fabricate long stroke diaphragms is to pre-stretch a fabric tube on a mandrel (A), creating a mesh that is stiff in the axial direction while permitting some radial expansion. The mesh is impregnated with Sylgard 170 RTV silicone to create a fabric that is stiff in the axial direction (B) but stretches in the radial direction (C). The final product shown in (D). |
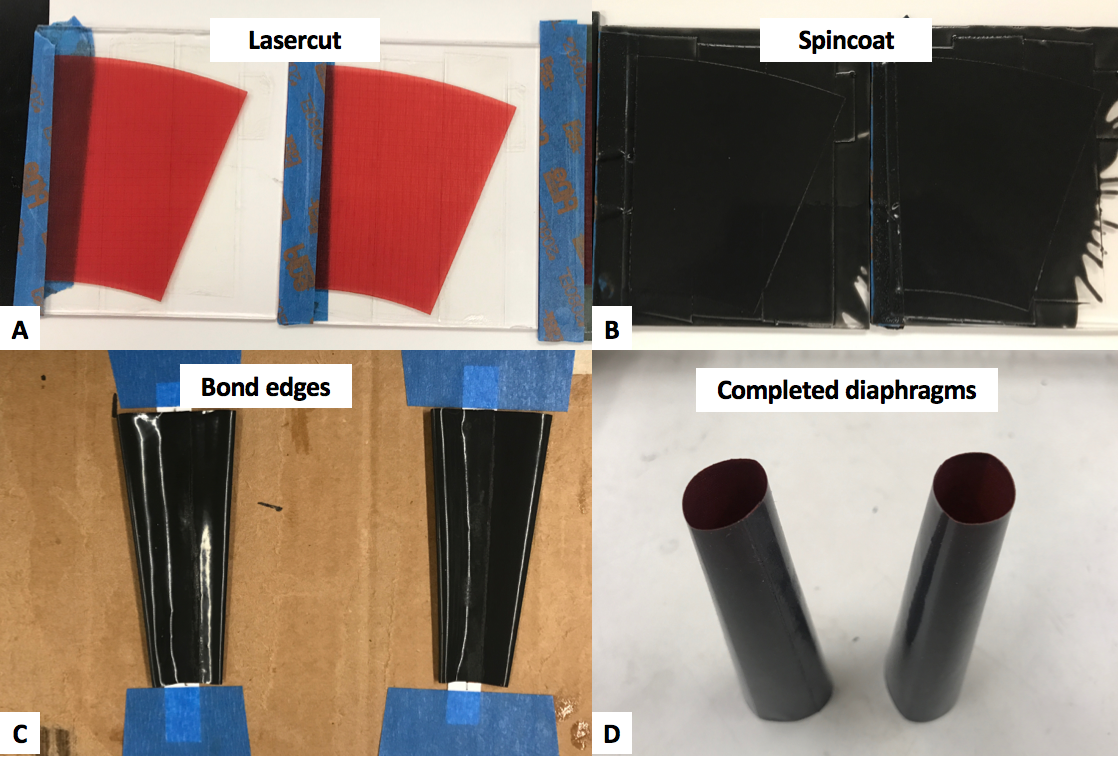 |
An alternative fabrication approach uses a thin ripstop nylon fabric (A) that is pre-impregnated with silicone. This fabric can be cut,coated with additional silicone (B) (Sylgard 170 RTV silicone at 600 rpm for 30 seconds) and rolled into a tubular shape (C). The final product is shown in (D). |
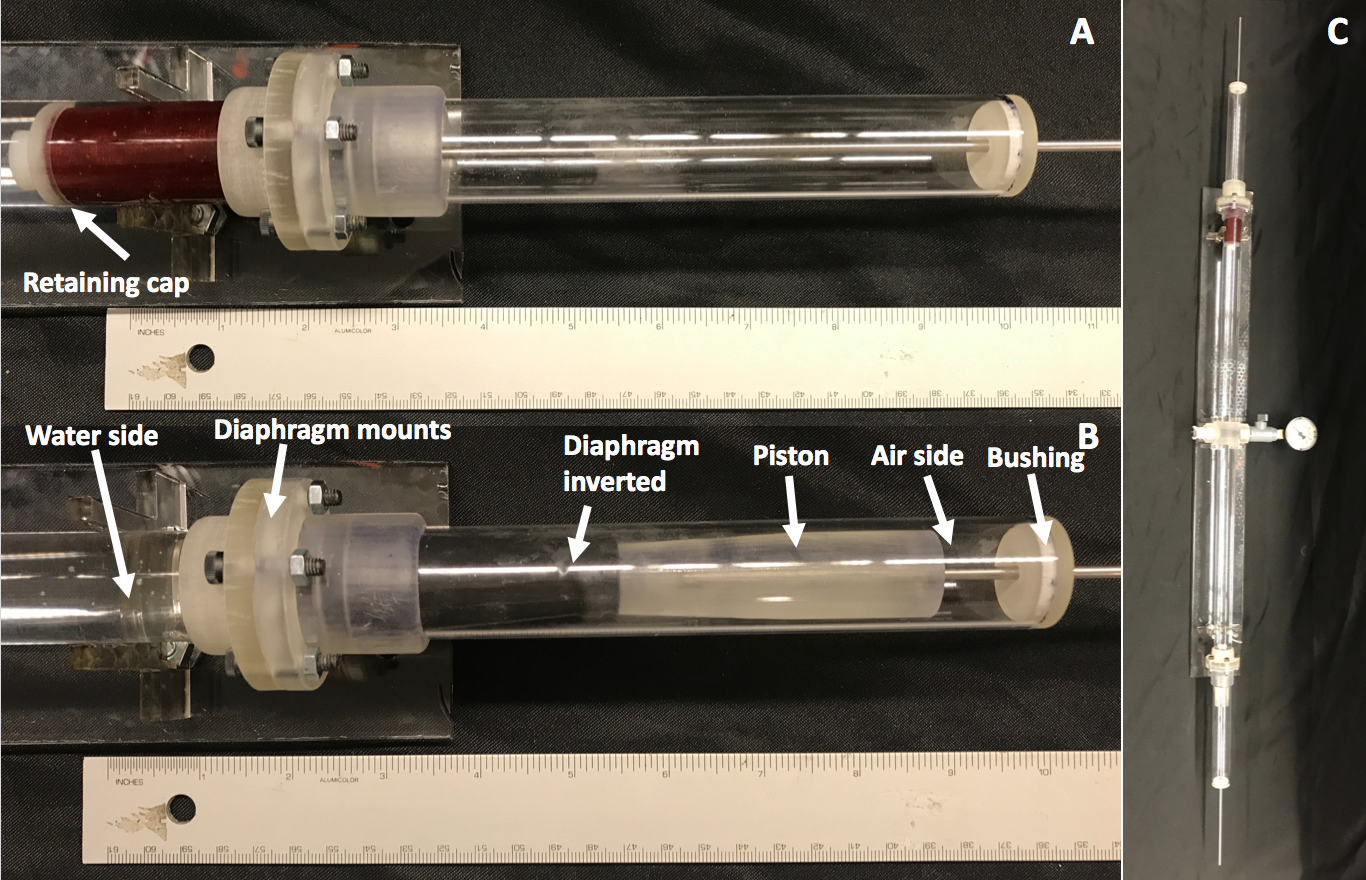 |
The silicone-impregnated-nylon coated rolling diaphragms have full stroke length of over 5.5 inches. If the pictured were the needle end of the system, (A) shows the diaphragm's position when the needle is fully retracted and (B) shows the position when fully inserted into a patient. The two diaphragms are connected back-to-back for testing with water in between (C) so that when one end is pushed, the other moves accordingly. Once fully inverted, the red silicone-nylon substrate is no longer visible (A,B). |
6. Research Team and Collaborations
- PI: Mark Cutkosky, Stanford University
- Graduate Students: Samuel Frishman, Natalie Burkhard, Alex Gruebele
- Collaborators:
- Genliang Chen, Shanghai Jiao Tong University
- Bruce Daniels, Stanford Radiology
- Peter Whitney, Northeastern University
- Funding
- This work is funded in part under NSF CHS:Small:Collaborative: #1617122 and #1615891 "Teleoperation with passive, transparent force feedback for MR-guided interventions"
7. Publications
Frishman, S., Kight, A., Pirozzi, I., Coffey, M.C., Daniel, B.L. and Cutkosky, M.R., "Enabling In-Bore MRI Guided Biopsies with Force Feedback," IEEE Transactions on Haptics (2020) 10.1109/TOH.2020.2967375
Gruebele, A., Frishman S. and Cutkosky, M.R., "Long-stroke rolling diaphragm actuators for haptic display of forces in teleoperation," accepted for IEEE RA-Letters, 2019. (preprint)
Burkhard, N., Frishman, S., Gruebele, A., Whitney, J.P., Goldman, R., Daniel, B.L., Cutkosky, M.R., "A rolling-diaphragm hydrostatic transmission for remote MR-guided needle insertion," IEEE ICRA 2017 (pdf). Best Robotics Paper Finalist